What is Inomyalgia? Defining the Term & Its Scope
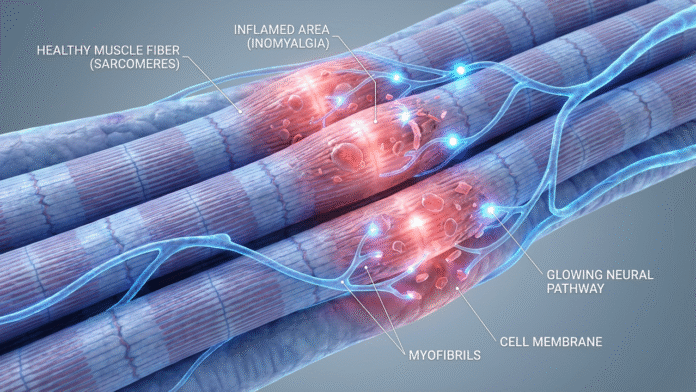
Inomyalgia appears to be a relatively new or emerging label used by some clinicians and chronic pain communities to describe persistent, deep-muscle pain and dysfunction that does not always fit classical diagnoses. The word is constructed from roots: “ino/ino-” (suggesting muscle fiber or internal muscle tissue) and “-myalgia” (meaning muscle pain).
Unlike simple myalgia which typically refers to transient muscle aches from overuse, injury, or viral illnesses inomyalgia is proposed to be more chronic, subtle, complex, and often not detectable via standard imaging or lab tests.
Because it remains less recognized than widely studied conditions such as Fibromyalgia, many patients with inomyalgia-like symptoms may go undiagnosed or misdiagnosed or labeled under “myalgia”, “chronic muscle pain”, or other broad terms.
Therefore, inomyalgia can be best understood as a descriptive, evolving term that’s used to explain muscle-based chronic pain, fatigue, and dysfunction particularly when conventional diagnoses fall short.
Symptoms & Patterns — What People with Inomyalgia Report
Patients or reports describing inomyalgia often highlight a cluster of persistent, fluctuating symptoms that can deeply affect quality of life. Commonly reported patterns include:
- Deep, persistent muscle pain or ache — sometimes dull, sometimes throbbing; often located in specific muscle groups or shifting over time.
- Muscle stiffness, tenderness or sensitivity — especially after mild exertion or when pressure is applied; muscles may feel tight, sore, or easily fatigued.
- Chronic fatigue and low energy — rest or sleep may not fully relieve exhaustion; muscle weakness and persistent tiredness are common.
- Sleep disturbances and non-restorative sleep — many report difficulty sleeping, waking up unrefreshed, or disrupted sleep cycles.
- Cognitive difficulties (brain fog) — reduced focus, memory issues, difficulty concentrating, sometimes associated with emotional or mental strain.
- Sensitivity to stress, temperature changes, or physical exertion — flare-ups may be triggered by environmental stressors, overwork, or even emotional stress.
- Mood disturbances, anxiety or emotional strain — due to chronic pain, fatigue, and often the “invisibility” of the condition, patients may feel misunderstood, isolated, or under-supported.
Because inomyalgia manifests variably from person to person in intensity, duration, and combination of symptoms it often presents a diagnostic challenge.
Why Inomyalgia Is Hard to Diagnose & Where It Stands Compared to Known Conditions
Absence of Standard Diagnostic Criteria
One of the most significant difficulties with inomyalgia is that, unlike established conditions such as fibromyalgia or recognized myopathies, there is no universally accepted diagnostic framework, no official classification in medical code sets.
Standard lab markers, imaging, or scans frequently appear normal because inomyalgia may involve muscle-fiber dysfunction, micro-trauma, neuromuscular sensitization, or other subtle mechanisms that evade routine detection.
As a result, diagnosis is usually by exclusion that is, ruling out other diseases (inflammatory myopathies, neuropathies, autoimmune disease, purely neurological causes), and then evaluating symptoms, history, physical exam, and response to treatments.
Overlap and Confusion With Other Pain Syndromes
Because many symptoms of inomyalgia pain, fatigue, sleep troubles, cognitive issues overlap with other syndromes like fibromyalgia, myofascial pain syndrome, chronic fatigue, or even psychosomatic disorders, confusion or mislabeling is common.
For example, while Myalgia is a generic term for muscle pain, it often refers to acute or transient muscle ache from overuse, injury, infection, or strain.
In contrast, inomyalgia implies deeper, longer-lasting, often disabling muscle pain potentially stemming from fiber or neuromuscular dysfunction rather than simple overuse or acute injury.
Similarly, compared with fibromyalgia which is widely studied and involves complex central nervous system pain processing often accompanied by systemic symptoms inomyalgia is sometimes described as more muscle-centric, fiber-centric, or tissue-centric, though the exact mechanisms remain debated.
Lack of Scientific Consensus & Evidence Gaps
Because inomyalgia is still an “emerging” or “alternative” classification in many sources, scientific research is limited. There is a lack of large-scale peer-reviewed studies, standardized criteria, validated biomarkers, or consensus guidelines. Some articles describe it cautiously as a hypothesis or working label rather than a formally recognized disorder.
This limited recognition can lead to underdiagnosis, dismissal by healthcare providers, or patients being told “there’s nothing wrong” which can worsen emotional distress and delay effective care.
What Causes Inomyalgia? Theories & Possible Mechanisms
Because inomyalgia isn’t yet formally established, its causes remain speculative or theoretical. However, across various articles and reports, several recurring factors emerge as likely contributors or risk modifiers:
- Muscle fiber stress, micro-trauma, or overuse — repetitive strain, overexertion, poor posture or chronic muscle tension can lead to internal muscle fiber damage, inflammation, or chronic soreness.
- Neuromuscular sensitization / central sensitization — similar to some chronic pain syndromes, the nervous system may become hypersensitive, amplifying normal muscle sensations into pain or discomfort.
- Neurochemical or hormonal imbalance — dysfunction in neurotransmitters (e.g. serotonin, substance P) or hormonal stress pathways may affect pain perception, muscle tone, or recovery.
- Psychological stress, emotional trauma or chronic stress — longstanding stress can manifest physically, increasing muscle tension, reducing healing capacity, and triggering or worsening symptoms.
- Mitochondrial dysfunction or impaired muscle metabolism — some newer theories suggest that energy production problems within muscle cells might underlie persistent fatigue and pain, even absent obvious inflammation.
- Lifestyle factors and environmental triggers — sedentary behavior, poor sleep, nutritional deficiencies, insufficient rest all can exacerbate muscle vulnerability and delay recovery.
Because of this complexity, many experts recommend adopting a biopsychosocial approach considering biological, psychological, and social factors together — to understand and manage inomyalgia.
Managing Inomyalgia: Best Practices & Recommendations
Given its unclear status and individual variability, managing inomyalgia often requires a personalized, multi-modal, holistic strategy. The goal is typically not a “cure,” but long-term symptom control, improved function, and quality of life. Here are key approaches commonly recommended:
✅ Physical Therapy & Graded Movement
- Gentle, low-impact exercises: stretching, yoga, swimming, walking helps maintain muscle flexibility and circulation without overloading.
- Progressive, graded movement: gradually increasing activity as tolerated can help avoid flare-ups while rebuilding muscle resilience.
- Posture improvement & ergonomic habits: since poor posture or repetitive strain may contribute, ergonomic corrections can reduce muscle stress over time.
🍎 Lifestyle, Sleep & Nutrition Adjustments
- Balanced diet rich in essential nutrients (vitamins, minerals, omega-3s) to support muscle metabolism, reduce inflammation, and promote recovery.
- Adequate rest and good sleep hygiene — since sleep disturbances worsen fatigue and inhibit healing.
- Stress management: practices like meditation, mindfulness, gentle breathing addressing psychological and emotional contributors to chronic pain.
💊 Medical & Supportive Therapies (As Needed)
- Pain management: depending on severity, medications like analgesics or muscle relaxants might be prescribed though efficacy varies and side-effects must be monitored.
- Multi-disciplinary care: working with rheumatologists, pain specialists, physical therapists, mental-health professionals to address the full spectrum of symptoms.
- Ongoing monitoring & evaluation: because inomyalgia may overlap with other conditions, continual reassessment (history, symptoms, triggers) helps tailor treatment and avoid misdiagnosis.
🧠 Psychological Support, Community & Self-Advocacy
Living with chronic, often invisible pain can be isolating and emotionally draining. Recognizing the legitimacy of one’s pain, seeking support through therapy or support groups and communicating needs clearly with loved ones and health professionals can significantly improve coping.
Why Inomyalgia Matters: The Case for Awareness & Acceptance
- Bridging a diagnostic gap: For many individuals whose pain doesn’t meet criteria for fibromyalgia or recognized muscle disease, “inomyalgia” may offer a more fitting description acknowledging real suffering even if standard tests are negative.
- Holistic understanding of pain: By considering muscle-fiber, neuromuscular, metabolic, psychological, and lifestyle factors together, the concept encourages a broader, more nuanced view of chronic pain beyond “just nerves” or “just muscles.”
- Reducing stigma and invisibility: Chronic muscle pain often leaves sufferers misunderstood. Recognizing inomyalgia helps validate experiences, promote empathy, and encourage support rather than dismissal.
- Encouraging research and better care: As awareness grows, more clinicians and researchers may examine muscle-based chronic pain potentially leading to better diagnostic tools, clearer criteria, and improved treatments for many currently underserved patients.
Conclusion: Inomyalgia A Working Concept for Real Pain
Inomyalgia may not yet be universally accepted or formally codified in medical textbooks. But it represents for many patients, caregivers, and forward-thinking clinicians a useful, compassionate, and honest attempt to name and understand persistent muscle pain and dysfunction that refuses easy classification.
By combining careful listening, broad-based evaluation, lifestyle and stress-aware care, and ongoing patient support, we can offer hope and manage inomyalgia more effectively even while the medical community continues investigating and refining its definitions.